1. Submit “balance bills” which will be negotiated for fair reimbursement
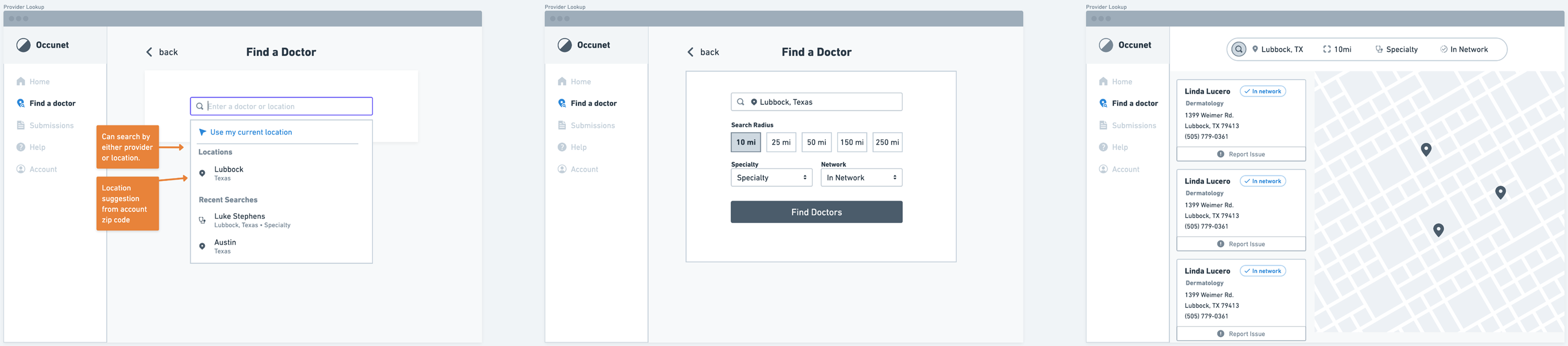
2. Find healthcare providers based on specialty, location, and whether they are in their network
.png)
.png)
The new search has resulted in 32% less searches without results and 48% more searches that result in a click. Members are able to find in-network providers quickly, and without worry or confusion over coverage.
Members are able to upload balance bills directly from their phone. This new process benefits both members by being able to manage their bill directly, quickly, and with added communication channels such as messages and notifications. This process benefits the business by reducing support and operational costs in contrast to how balance bills were handled previously.
For this project, Fairos conducted their own research (Surveys, Interviews, Analytics) that gave us some early insights on issues to address.
Through a collaborative ideation process involving myself, product, and another designer, an approach of outcomes and solutions were identified and proposed to stakeholders. Our main goal was to keep the provider search journey inside the portal up to the point of provider contact, and Offers more usable search experience that results in less searches without results and more searches that result in a click.

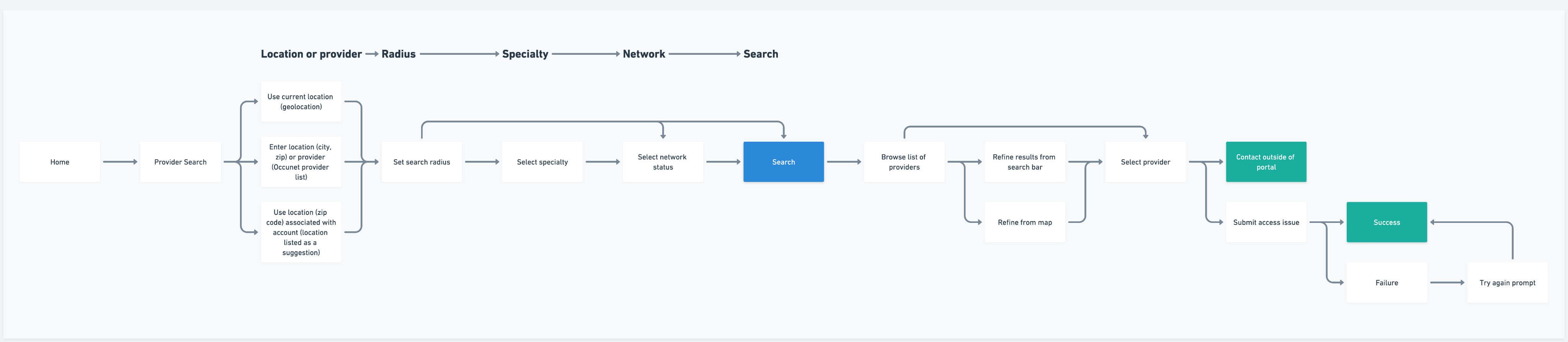
Following aligning internally and externally around our flows, we moved on utilizing wirefaming to map out the new experience. This phase held the most collaboration as we used this time to truly align visually, determine feasibility, and iterate accordingly.
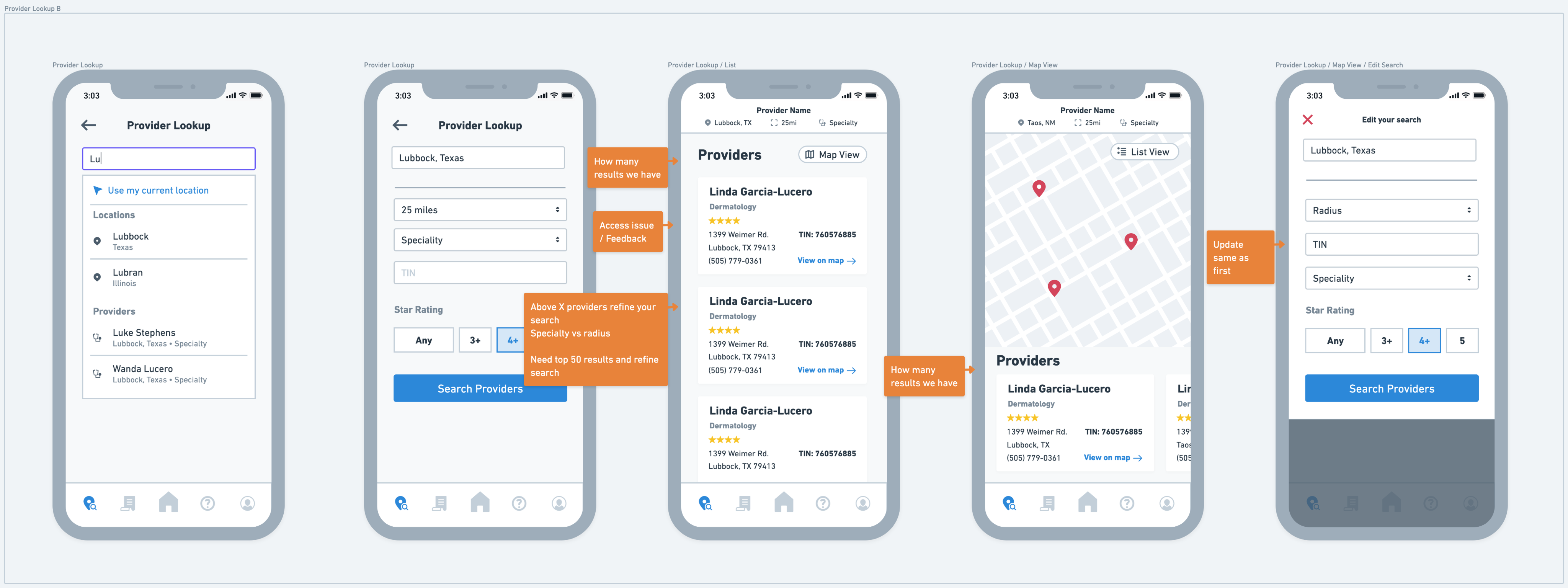
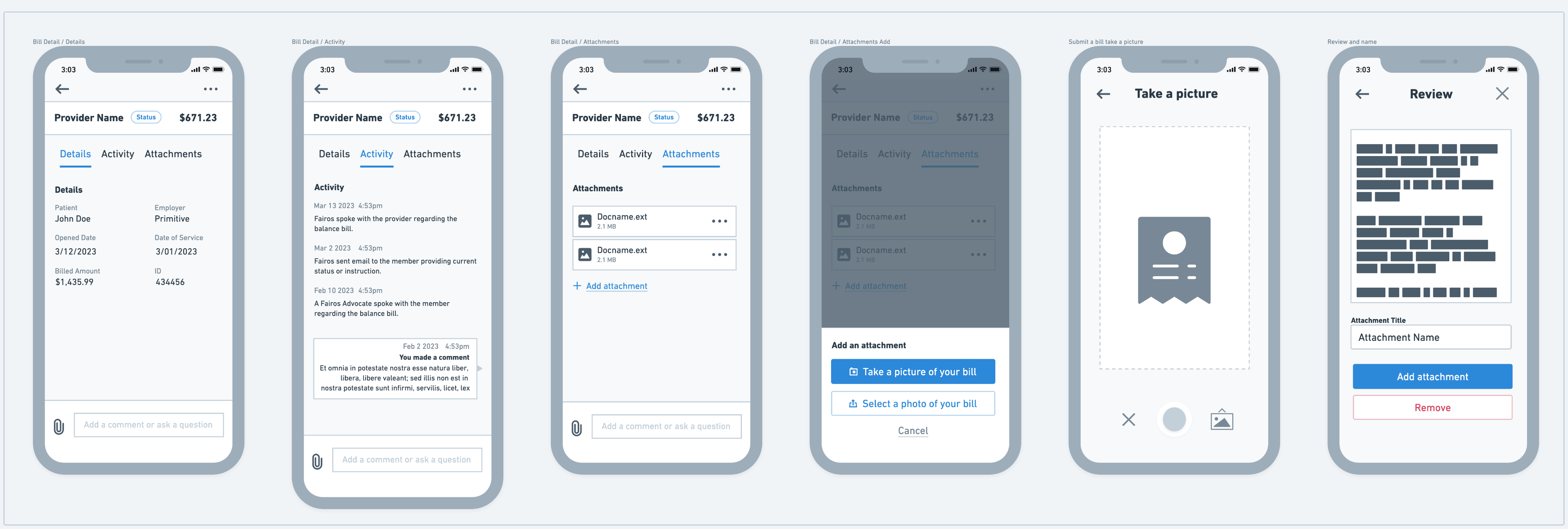
In this phase, we were able to take our business objectives, user needs, and proposed solutions contained within the wireframes and bring them to a higher fidelity, ultimately ending with a clickable prototype delivery. We used Figma as the primary tool for the UI design + prototype.
.png)
.png)
.png)
A design system and style guide was developed and maintained by our team in order to increase alignment with external teams and to keep the design consistent and effecient as it scaled. The design system documented:
.png)